8 Warning Signs for Impacted Wisdom Teeth & 4 Impaction Type


Think you might have impacted wisdom teeth? These impacted third molars are more common than you think, with most people having at least one impacted wisdom tooth.
In the typical mouth, each of us has a total of four wisdom teeth. There’s one at the very back on either side of our upper and lower arch of teeth. Although, some people have congenitally missing wisdom teeth or supernumerary (extra) ones!
What Are Impacted Wisdom Teeth?
In the perfect world, our third molars (wisdom teeth) would erupt right into place just like all of our other teeth did before them. Unfortunately, these molars are statistically at a high risk of becoming “stuck” or “impacted” inside of the jaw.
An impacted wisdom tooth is any third molar that is somehow physically wedged down under the gum tissues or bone. As a result, it fails to erupt properly.
Impacted wisdom teeth may be completely wedged down inside of the jaw or only erupt by a small amount.
Since the wisdom teeth are the last set of molars to develop—the previous ones erupt around ages 6 and 12, respectively—they tend to be seen as a “rite of passage” into adulthood. Usually, by the age range of 14-16, we know whether or not a wisdom tooth is going to be impacted and if it will need to be removed.
8 Impacted Wisdom Teeth Symptoms
What are the signs and symptoms of impacted wisdom teeth?
1. Nothing at all
In this case, you don’t even realize you even have wisdom teeth. They don’t hurt. There’s no swelling. You probably don’t even know they’re there until your dentist takes an X-ray.
2. Sore gums, mouth, teeth, or jaws
The pressure that’s created by impacted wisdom teeth can make your mouth hurt or sore in general. Think about the “teething” pain that infants experience; there’s a reason why they’re so fussy!
3. A bad taste in your mouth
Partially impacted wisdom teeth are highly prone to infections, which can leave a foul or sour taste coming from that space.
4. Bad breath
Just like the point above, partially-erupted wisdom teeth may have odorous bacteria lurking around them, which can impact the way your breath smells.
5. Swelling
Facial swelling, jaw swelling, and swollen gums are extremely common around impacted or partially impacted wisdom teeth. In some cases, the swelling is noticeable to other people or severe enough that it limits the movement of your jaws (like when you’re chewing or yawning.)
6. Crowded teeth
Impacted wisdom teeth may be pressing on the teeth that are next to them. This pressure can physically move your teeth the same way braces would. Normally all of that movement presents itself as crowded teeth in the front of your smile.
7. Fever
If you have partially impacted wisdom teeth that are severely infected, you might develop an elevated temperature.
8. Cysts
Every tooth has a natural “eruption cyst” around it. But when it erupts, it usually goes away. Impacted molars may have a large and atypical cyst around them, which can cause damage within the jawbone.
Fully Impacted Wisdom Teeth
With a fully impacted wisdom tooth, the only way for your dentist to examine it is with a panoramic X-ray or CBCT scan.
Since wisdom teeth typically erupt during the mid to late-teen years, you’ll probably know if you have a fully impacted wisdom tooth well before you head off to college. But if you haven’t seen a dentist as a teen and now you’re an independent adult—and there are no visible wisdom teeth in your mouth—they’re likely either fully impacted or completely missing.
Partially Impacted Wisdom Teeth
Partial impaction allows food and bacteria to seep down under the gums, lodging itself around the tooth underneath. That’s why they’re such a big issue, even if your tooth doesn’t hurt any. They’re basically a ticking time bomb for cavities and periodontitis.
Non-Impacted Wisdom Teeth
Are there ever situations where wisdom teeth don’t get impacted?
YES!
Sometimes wisdom teeth erupt completely normally into the mouth. Or they get pretty close to it, with just a small amount of soft tissue overlapping them. They’ve erupted enough to chew with, anyway.
The biggest downside to erupted wisdom teeth is that they’re so far back in your mouth. Oftentimes, space limitations prevent adequate brushing and flossing (no matter how hard you try.) Unless you’re using a water flosser around them 4-5 times a day, these teeth are highly likely to develop cavities and/or gum disease. And both of those infections can spread to the neighboring tooth.
4 Types Of Impacted Wisdom Teeth
There are several different positions and directions that impacted wisdom teeth can find themselves in.
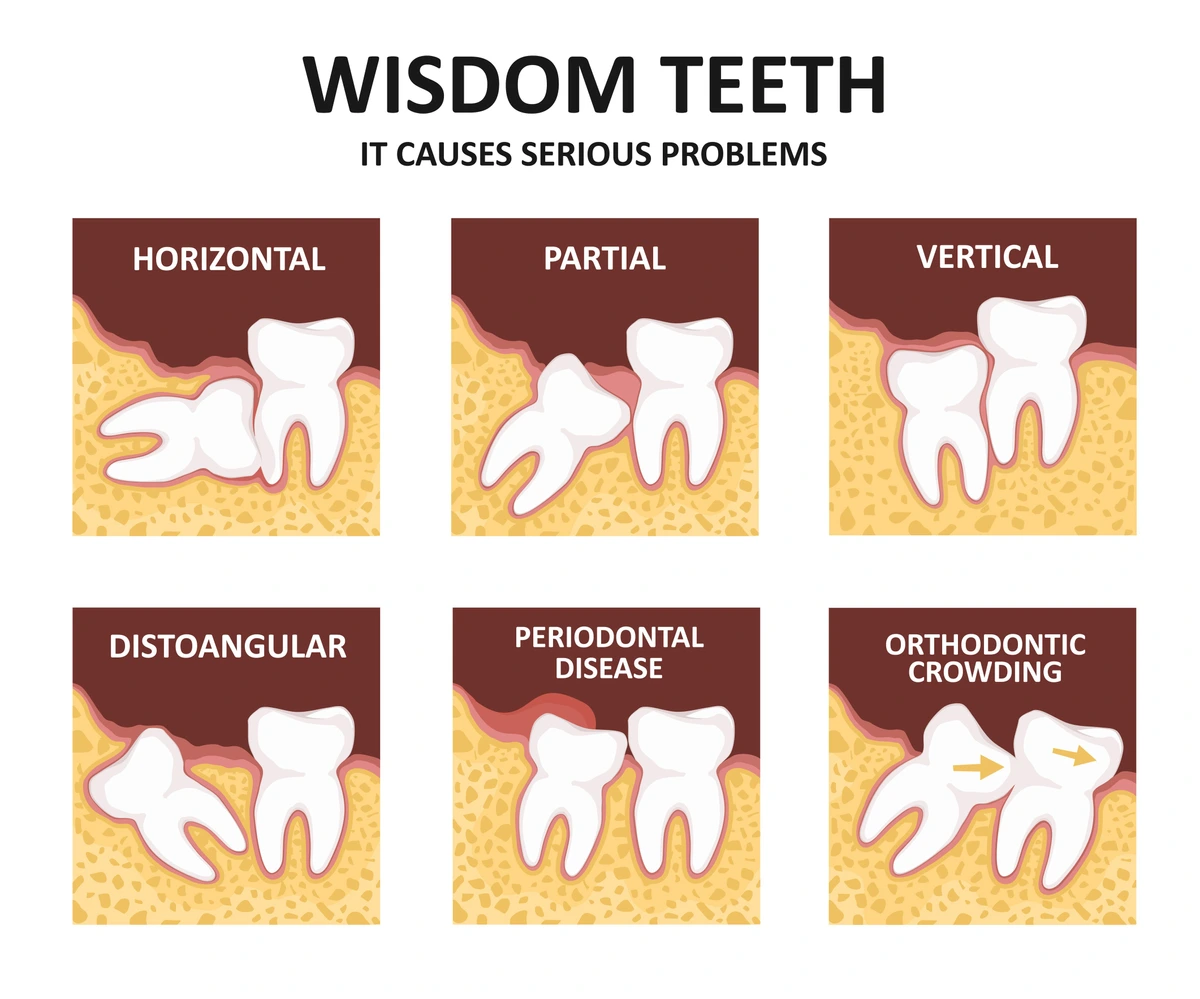
1. Mesial Impaction
Sometimes called “angular impactions,” a mesial impaction is where the developing wisdom tooth is angled mesially, that is, toward the “midline” or middle of the mouth. It’s usually tilted into the adjacent tooth rather than positioned vertically like the rest of your teeth. These are the most common types of impacted wisdom teeth to have.
2. Distal Impaction
If you’ve ever looked at a full-mouth dental X-ray and seen the wisdom teeth (at the very back of the mouth) angled backward and away from all of the other teeth, this is a distal impaction. They are trying to erupt distally (away from the midline) and thereby become wedged inside of the jaw. It’s physically impossible for these teeth to erupt.
3. Vertical Impaction
A wisdom tooth that is vertically impacted can seem a little confusing to some. Typically it is situated straight up and down, just like the next tooth is, but it doesn’t have the ability to erupt through the soft tissues and into the mouth.
4. Horizontal Impaction
Whenever a wisdom tooth is horizontally impacted, it is essentially laying completely sideways in your jaw, perpendicular to the other teeth. As it grows, it presses back into the bone and nerve area as well as straight into the tooth in front of it. These wisdom teeth typically cause pain, damage to the neighboring tooth, and lead to crowded teeth at the front of your smile.
Soft Tissue Impaction vs. Hard Tissue Impaction
There are two different levels of impaction a wisdom tooth can have.
The first is a soft tissue impaction. These scenarios are where the wisdom teeth are fully or partially covered with soft gingival tissue (aka your gums). Soft tissue impactions usually cause swelling, soreness, and redness in those areas because of the pressure that’s created. Although they have erupted through the bone, they don’t “come in” through your gums.
The second is hard tissue impaction. This is where the impacted molars are wedged against a hard structure, such as a portion of the jawbone/mandible or the roots of adjacent teeth. Left alone, the pressure of an impacted wisdom tooth could lead to resorption (shrinkage) of those hard structures.
Normally, removing a wisdom tooth that has a soft tissue impaction is less invasive than those suffering from a hard tissue impaction. But hard tissue impactions are still fairly common and easily managed by a board-certified oral surgeon.
What Causes Impacted Wisdom Teeth?
While we don’t necessarily know why wisdom teeth are automatically impacted for most people, we can hypothesize about some of the scenarios that might make certain people more prone to impaction.
For example, since most of us have access to preventative dental care, we’re keeping our natural teeth longer than ever. And that’s a great thing! We aren’t losing them because of decay or gum disease in our 30s.
But there’s also a consequence of that. Since there aren’t any missing teeth, the wisdom teeth don’t have any extra space to fill in once they erupt. So they tend to become lodged against adjacent teeth or the bone.
Are Impacted Wisdom Teeth Common?
Yes. According to the American Academy of Oral and Maxillofacial Surgeons, 9-in-10 of us will experience impacted wisdom teeth in our lifetimes. In other countries, those statistics will vary, depending on facial anatomical characteristics and genetics. Studies in Europe have reflected similar statistics, although it was a bit closer to 3-in-4 adults being affected.
People who are less likely to experience impacted wisdom teeth often include Asians and people of African heritage, as those demographic groups are known for statistically having fewer than four wisdom teeth compared to people of European descent.
How Are Impacted Wisdom Teeth Treated?
The only two options for treating impacted wisdom teeth are to surgically remove them or do nothing at all.
Surgical wisdom tooth removal can range from simple to complex. Some people are able to have their wisdom teeth removed with only a small amount of local anesthetic to numb their teeth, while others prefer a strong sedation medication to “knock them out” as the area is accessed by the oral surgeon.
As scary as oral surgery sounds, removing impacted wisdom teeth is something that oral surgeons specialize in and do almost every day of their career.
Leaving your impacted molars in place is only recommended in certain situations. Particularly when they are not pressing into neighboring teeth or against the nerve in that space. In most scenarios, these molars are labeled with a “watch” by your dentist so that they make a point to re-assess them at every checkup. You won’t want to leave them there if they start to develop an infection or cause pain.
Complications Of Surgery
As with any type of surgery—be it medical or dental—there are possible complications and side effects that can occur. Although complications of removing impacted molars are rare, they do still exist. Here are some of the most likely scenarios you’ll want to ask about before signing your consent form before surgery:
1. Dry socket
This is where the blood clot comes loose or dislodged after your wisdom tooth removal. It delays the healing time and is usually extremely painful for at least a couple of weeks. Dry sockets are the most common complication of wisdom tooth removal.
2. Nerve damage
3. Damage to other teeth
Depending on how badly impacted wisdom teeth are, there is a potential for the adjacent tooth to be damaged during the removal process.
4. Jaw fracture
Severely impacted teeth that are embedded within the bone may result in bone fractures during removal.
Dealing With Impacted Wisdom Teeth Pain
Pain from impacted wisdom teeth tends to come and go. It might be steady for several days, then let off, then come roaring back. Unfortunately, this cycle is normal until you have your impacted molars removed. But in the meantime, there are some things you can do to help manage your discomfort.
First, take an anti-inflammatory. Motrin or ibuprofen is usually best. These medications help reduce swelling, which is a common side effect of impacted molars or adjacent infections around your wisdom teeth.
Second, apply a cold compress onto that side of your mouth for 15-20 minutes at a time. The cold temperature will also help with swelling and numb the pain.
Rinsing with warm salt water a few times a day can also be beneficial.
Is It Necessary To Remove Impacted Wisdom Teeth?
Usually, partially-impacted or fully-impacted wisdom teeth need to be removed. Not just because of the pain they cause, but because of the risk of dental problems they pose to the rest of your smile. Without removing your impacted molars, they can lead to permanent damage in adjacent teeth, whether from infection or decay, and cause significant crowding throughout your smile.
Do All Wisdom Teeth Need Extracting?
Your specific oral anatomy will impact whether or not you need to have your wisdom teeth removed. If you have a slightly larger jaw where there’s plenty of room for everything to line up nicely, you may not need them removed at all.
When To Talk With Your Dentist
Usually, most dentists perform a wisdom tooth evaluation on a patient by the time they’re about 15 or 16 years old. Then they may “keep an eye” on them until they’re well into their 20s if wisdom tooth removal isn’t needed.
Adults and teens should talk to their dentist about any symptoms of wisdom tooth pain, jaw soreness, swelling, bad taste in their mouth, or a foul odor coming from that area.
Listen. You don’t need to stress about this visit with your dentist. All they’re going to do is get you in for an exam and either take a panoramic X-ray or a 3D CBCT scan. Then they’ll talk to you about what they see and what your options are.
What To Do About An Impacted Wisdom Tooth?
Impacted wisdom teeth are common in most teens and adults. Sometimes these impacted third molars can be left alone, while other times, they press into and damage adjacent teeth. Proactive removal can help with managing pain and preventing the unnecessary risk of infection in the future. Ultimately, everyone’s smile is different. It’s up to you to see your dentist regularly to monitor your wisdom tooth development and decide if extracting them is right for you. Unless there is perfectly enough space and you can brush and floss around them effectively, you’ll probably want your wisdom teeth removed regardless.
Make your inbox smile!
Subscribe