5 Stages Of An Abscessed Tooth & What To Do


What does a tooth abscess look like? To some people, an abscessed tooth may look like a gum abscess. Stages of the infection vary, with symptoms fluctuating depending on how long you’ve had an abscessed tooth, how “bad” the bacterial infection is, and the extent of the tooth deterioration. Although it’s possible to treat abscessed teeth, the actual tooth abscess stages will eventually reach a point where it’s physically impossible to repair or save your anatomical tooth.
What is a Tooth Abscess?
Every tooth has a living, functional nerve and blood vessels that run down the center of the root. The nerve is responsible for “feeding” your tooth structure and keeping it alive. But if that nerve or tissue supply is somehow compromised or infected, you’ll develop a periapical abscess.
Gingival Abscess (Gum Abscess)
Scientifically speaking, it’s possible to get an abscess practically anywhere in our body. In the case of a gingival abscess, the infection is strictly localized inside of our gum tissues (and not the tooth itself.) This could be due to some type of oral infection, medical condition, trauma, or lack of home care.
Periodontal Abscess
If you have severe periodontal (gum) disease, the gum and bone tissues adjacent to your tooth roots become severely infected. Although traditional symptoms include pocketing, tartar buildup, and bad breath, some people may also develop periodontal abscesses where fluid drains out of the gums when pressure is applied to the tooth.
Periapical Abscess
These are the most common types of dental abscesses. They are the result of an infected or dying tooth nerve, with a developing cyst at the tip of the tooth root that ultimately drains through the gums and into the mouth. Periapical abscesses can only be managed with endodontic therapy.
What Does An Dental Abscess Look Like?
Depending on the type of dental abscess you have, you’ll usually experience symptoms of swollen gums, fistulas (small pimple-like sores) on the tissue, and even visible pus that drains from that location. If you have a periapical abscess, the cyst around the root will usually be visible on a dental x-ray. Abscesses within the gums typically accompany red, inflamed tissues that bleed easily and are tender to touch.

It’s extremely common for tooth abscesses to “come and go”, with visible symptoms for a few days and then gone the next. Whereas if it’s simply something like an ulcer, the blister tends to appear on otherwise completely healthy gum tissue and heals within a week or two.
5 Dental Abscess Stages
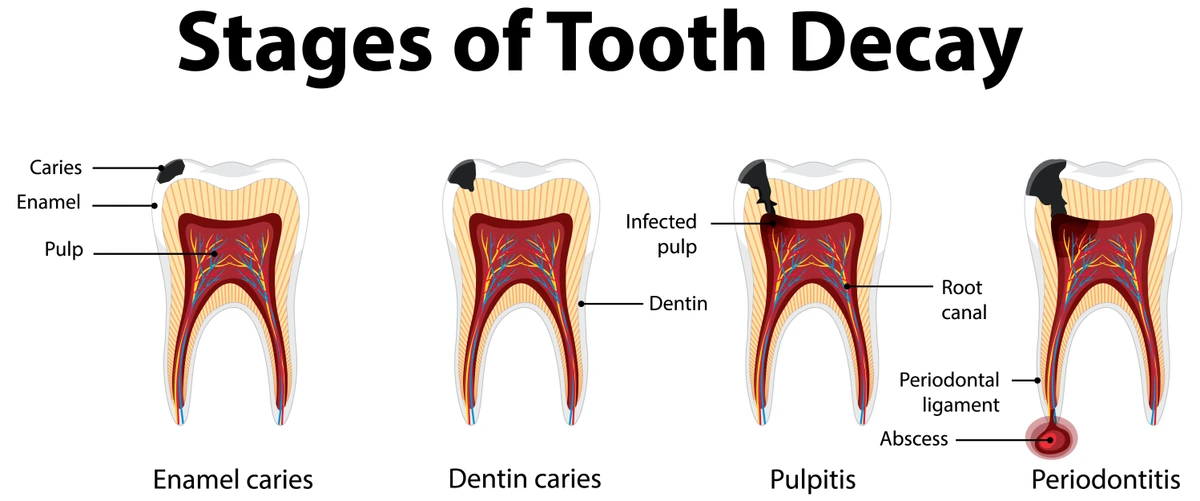
1. Enamel Decay
Aside from traumatic injuries, almost every abscessed tooth is the result of enamel decay. The outermost layer of your tooth is made of extremely dense enamel. Once a cavity has begun to erode your tooth enamel, it is fast on its way to becoming an abscessed tooth…unless you treat it ASAP.
Symptoms
Not all cavities have noticeable symptoms. But the most obvious ones include sensitivity, pain, darkening of your tooth enamel, rough edges, and visible holes in your teeth on your dental X-rays.
Treatment
2. Dentin Decay
Underneath the enamel is a layer of the tooth called dentin. Dentin is much less dense than enamel, so once a cavity reaches this layer it can spread at alarmingly fast rates. The dentin is the bulk of the tooth surrounding the inner nerve tissues. Dentin decay also tends to be much more sensitive than enamel.
Symptoms
Once a cavity reaches into the dentin, your tooth will likely be far more sensitive. You might notice something feeling “off” whenever you chew. Floss will usually get caught whenever you’re cleaning around your tooth if the cavity is between teeth. There’s also a high risk of the tooth breaking whenever you bite down.
Treatment
A dental filling, inlay, onlay, or crown will be necessary depending on how much tooth structure is involved. Without treatment, an infected pulp is inevitable.
3. Pulp Decay
After a cavity has ruptured the tooth enamel and spread into the dentin, it is only a matter of time before the decay reaches the nerve in the middle of the tooth. Once active decay contaminates the pulp/nerve tissues, the entire tooth becomes compromised. Unless treated immediately, tooth loss is inevitable.
Symptoms
Once the pulp tissue inside of a tooth is infected, sensitivity to hot foods and drinks is common. More than likely, teeth will be hypersensitive to everyday activities like eating, drinking, and brushing your teeth. Sharp or dull toothaches are common.
Treatment
The only treatment for an infected pulp tissue is endodontic therapy. During a root canal, the nerve is removed and the chamber is sealed off with a special filling material to prevent bacteria from re-entering the canal. You’ll also need a crown on top of the tooth. For children, a pulpotomy (“baby root canal”) is usually the best alternative.
4. Dental Abscess Formation
Shortly after decay reaches the tooth nerve, bacteria become trapped inside of the pulp chamber. This leads to deterioration of the nerve, development of a pocket of pus, and a rise in inflammation. There are only two directions for the tooth infection to drain, and one of them is through the opening at the tip of the root.
Symptoms
Shortly after the nerve of a tooth becomes infected, the inflammation will lead to excess fluid that needs to drain out of the tooth. A fistula—or small pimple on the gums—allows pus to drain through the bones and gum tissue to ease the pressure inside the root. As the tooth begins to die, it will gradually turn dark and become more brittle. There could be severe tooth pain or none at all (because the nerves are no longer functioning properly.)
Treatment
Root canal treatment will eliminate the source of the tooth abscess, and prevent total tooth loss as well as additional discomfort.
5. Serious Complications
An untreated tooth abscess can easily expand into adjacent anatomical structures. In some cases, these have been known to cause brain infections, facial swelling, and require hospitalization. Loss of the tooth is common, as is an infection in adjacent teeth.
Symptoms
Treatment
You will require hospitalization and intravenous drug treatment to gain control over systemic infections throughout the bloodstream and secondary organs. Once your medical condition is stabilized, the tooth is extracted.
Symptoms of a Dental Abscesses?
It’s really important to know that tooth abscess symptoms can vary from person to person. But in a broad sense, here's what you can usually expect to see or experience at some point:
Early tooth abscess stages:
- Sensitivity
- Tooth pain
- Tooth decay, cracked teeth, or gum disease
- Enlarged nerve on your dental X-ray
- Darkening around the root of your tooth (as seen on your X-ray)
Late tooth abscess stages:
- A bad taste in your mouth
- Visible pus draining from somewhere around your tooth
- The tooth moves when pressure is applied
- Darkening of your tooth
- A fistula (pimple) on the gums next to the tooth root
- Swollen or red gum tissues at that area
What Causes Dental Abscesses?
Almost all dental abscesses are the result of untreated tooth decay. Since cavities are a bacterial infection, they continue to expand into adjacent tooth structures unless they’re physically treated by your dentist.
Deep cracks in teeth can also contribute to an abscessed nerve. For instance, if a traumatic injury during an athletic event or car accident involves blunt trauma to the mouth, it could fracture the tooth and allow bacteria to enter the nerve chamber.
Untreated gum disease can also cause periodontal (gum) abscesses. These infections are caused by a lack of regular preventative care, heavy tartar buildup underneath the gum tissues, and inadequate brushing and flossing.
Unfortunately, a lot of people assume that if their tooth doesn’t hurt or there isn’t anything visibly wrong with it, they don’t need to treat the cavity or crack. So, this allows the condition to go untreated, meaning more and more bacteria can enter the tooth.
Early screenings, regular dental exams, and diagnostic digital X-rays can eliminate the cause and progression of a dental abscess. Sadly, a lot of people just don’t listen to their dentist’s recommendations regarding abscessed teeth, especially when there isn’t any noticeable pain.
Dental Abscess Treatments
How to treat a tooth abscess? Depending on the type of dental abscess you have and its severity, you’ll need one of the following treatments:
1. Antibiotic
Wait…what?! I know what you’re thinking. I already said that you couldn’t treat an abscessed tooth without some type of restorative procedure. And you can’t. If the tooth infection has spread, antibiotics can reduce the inflammation and level of bacteria inside that area so that your dentist can comfortably numb the tooth to remove the source of the infection. If there’s severe swelling, the numbing medication won’t work well. But you can’t take antibiotics to get rid of a tooth abscess like you would for something such as strep throat.
2. Endodontic Therapy
Root canal treatment is usually the only option if you have an abscessed nerve. It’s essentially removing the nerve, cleaning out the canal, and then sealing off the chamber to prevent reinfection. Simply covering over the tooth with a filling or crown won’t fix the issue; all it will do is trap the infection inside of your tooth.
3. Scaling and Root Planing
For periodontal (gum) abscesses, the infection is in the gums or bone next to your tooth, and not the tooth nerve itself. When that’s the case, we need to clean out the bacteria causing the infection. Normally, it’s due to tartar and plaque wedged deep under the gums next to the tooth. In those scenarios, a “deep cleaning” is prescribed.
4. Tooth Extraction
In really severe situations, if the tooth abscess is overtaking your tooth, and there is no way to save the tooth, tooth extraction may be your only treatment choice. By then, you’ll also need to come up with a way to replace the tooth shortly thereafter.
Risk Factors of an Untreated Dental Abscess
Not to scare you or anything, but in a total worst-case scenario, untreated tooth abscesses can allow infection to spread into your face and your brain. There are actually documented cases where untreated dental abscesses resulted in death. This scenario is a big issue in children especially when abscessed baby teeth aren’t treated in a timely manner.
Thankfully, early dental care keeps most people out of the hospital. But if you try to avoid trips to the dentist’s office, most untreated abscesses typically lead to painful emergencies and tooth loss.
Tooth loss is usually the result of the tooth abscess getting so bad, that there’s not enough structure that’s left to restore. At that point, your dentist’s hands are tied and the only way to totally eliminate the tooth infection is to pull the tooth entirely.
Or you lose your tooth because of the throbbing pain. If you need short-notice emergency treatment, tooth extraction can provide a fast way to totally eliminate the source of the infection. Especially if you’re dead-set against a root canal treatment.
But with tooth loss comes a whole plethora of additional issues. Like displacement of other teeth, because they start to tilt and drift out of alignment when one of their partners goes missing. As teeth start to move out of place, it contributes to TMJ issues, irregular wear patterns, bone loss, and future expenses related to tooth replacement.
Can A Tooth Abscess Go Away On Its Own?
When we get sick, we take medicine, stay hydrated, rest, and “wait it out.” But there are certain types of infections and diseases that just don’t improve with rest and relaxation. Tooth decay and abscessed teeth are one of them.
The longer you wait, sure, you might notice the pain start to go away. But that’s probably because the nerve of the tooth is starting to die, taking the pain receptors right along with it.
Ultimately, untreated tooth abscesses will only get worse and eventually lead to tooth loss. If you’ve ever heard someone say they healed an abscessed tooth on their own, they didn’t truly have a periapical abscess to begin with, or there’s still an infection that they don’t know about.
Preventing Dental Abscesses
Prevention is the best medicine in the world. Especially when it comes to your smile. By practicing good everyday oral hygiene habits—including brushing along the gumlines and flossing every single tooth every single day—and scheduling regular dental checkups, you can almost totally eliminate your risk of an abscessed tooth.
But what about the abscesses caused by cracked teeth? In those scenarios, it’s best to wear a protective mouthguard (sports guard) during any type of physical activity where oral trauma may occur. Not only can a great-fitting sports mouthpiece protect your teeth, but it can also safeguard your brain against a concussion.
Always make a plan to see your dentist and hygienist every six months for a checkup. They’ll thoroughly clean your teeth and screen for early warning signs of decay. By preventing gum infections and cavities before they start, you can save your smile AND your wallet.
Talk To Your Dentist
And if you don’t feel comfortable with a dentist’s recommendations to get a root canal or deep cleaning, always seek out a second opinion. It’s better to be cautious than ignore a potentially abscessed tooth. In most cases, a second opinion visit is covered by your insurance, because your carrier knows you’re probably going to go with the more conservative of the two.
Try not to wait for more severe tooth abscess stages before seeking out a professional opinion. See a dentist at the earliest inkling that there’s something wrong with your tooth.
Stages of Abscess Tooth
Tooth and gum abscess stages vary, depending on the type of dental abscess you have. But one thing is for certain, you need to get it treated quickly. What does a tooth abscess look like? Usually, a swollen blister or pimple on your gums, with pus that drains from that area. Some abscesses cause fluid to drain out near the gumlines whenever the tooth is depressed. The earlier you seek out professional care, the better chances you have of saving your tooth and preventing the infection from spreading elsewhere. Don’t ignore abscessed teeth; in rare conditions, they can put you in the hospital because of how life-threatening the infection is.
Make your inbox smile!
Subscribe