9 Causes Trigeminal Neuralgia & Avoiding Triggers


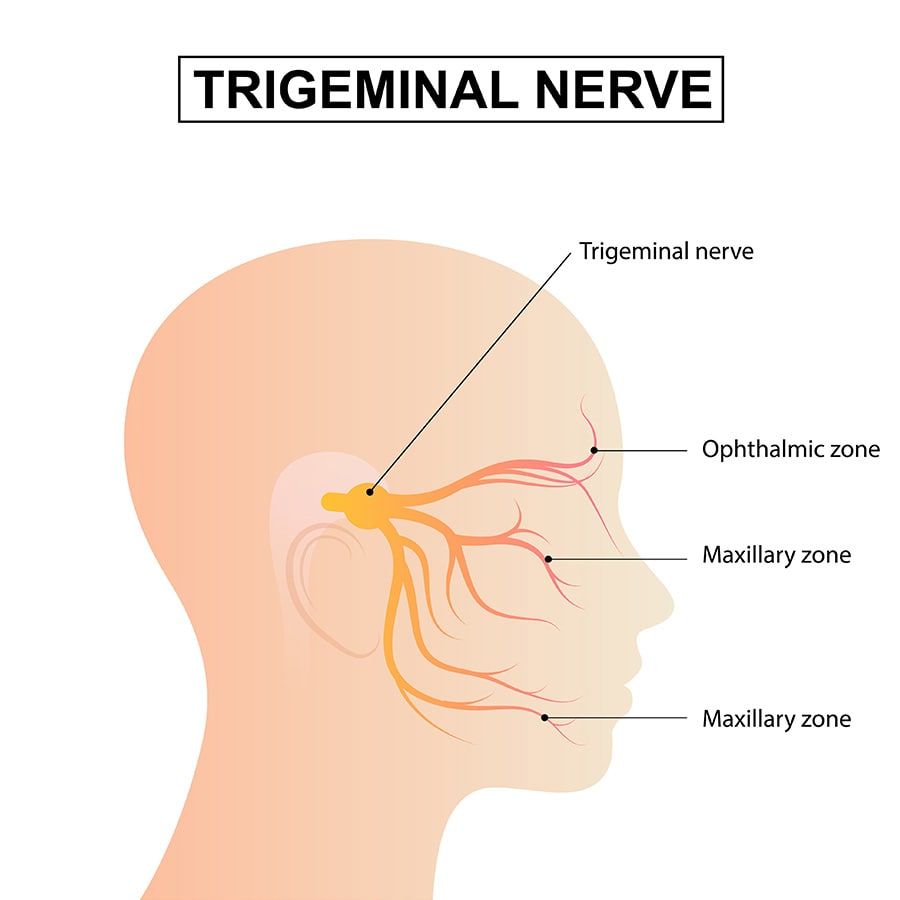
The trigeminal nerve is one of the largest nerves in our head and face. It’s responsible for transmitting sensations from various parts of our face to our brain. It is divided into three branches (hence the “tri” in its name,) each of which supplies different regions of the face, including the forehead, cheeks, and jaw. The nerve is also involved in managing the physical motor function of our jaw muscles, allowing us to do important things like chew and bite into our food.
In addition to its sensory and motor functions, the trigeminal nerve plays a role in important reflexes, like blinking our eyes, to prevent injuries.
Part of the trigeminal nerve runs alongside our jaw and face. But neurological injuries can cause chronic pain or inhibit signals between this important nerve and the brain. Trigeminal neuralgia is one classic example.
What Is Trigeminal Neuralgia
Trigeminal neuralgia is a neurological (nerve) condition that causes severe, stabbing, or electric shock-like pain in the face, typically on one side. It's caused by irritation or damage to the trigeminal nerve, which is responsible for transmitting sensations from the face to the brain.
Trigeminal neuralgia pain can be triggered by even the lightest stimuli, such as eating, talking, or a light touch to the side of the face, and can feel extremely debilitating.
While the exact cause of trigeminal neuralgia is not always known, it can sometimes be associated with conditions such as multiple sclerosis, tumors, or blood vessel abnormalities.
It's important for dental patients with trigeminal neuralgia to communicate their health history and any medications they’re taking to their dental provider(s.) This can help ensure that their oral health care plan is tailored to their individual needs and takes into account the impact of trigeminal neuralgia on their dental health.
Trigeminal Neuralgia & Dental Problems
Trigeminal neuralgia can affect a dental patient and their oral health care plan in several different ways. For example, if the pain is triggered by certain stimuli, such as eating or brushing teeth, the individual may avoid these activities altogether. When that happens, it can lead to inadequate oral hygiene and a seriously increased risk of dental problems like tooth decay and gum disease.
Some of the medications that doctors use to treat trigeminal neuralgia symptoms can also cause dry mouth. But a lack of saliva can also increase the risk of dental problems. Especially since saliva helps to wash away food particles and neutralize acids that cause tooth decay. Because of that, dental patients with trigeminal neuralgia may need to take extra care to promote good oral hygiene. Such as considering using products that help combat dry mouth and reduce the risk of cavities.
Unfortunately, certain dental procedures like extractions or restorative work may trigger pain in patients with trigeminal neuralgia. In these cases, the patient and dental professional may need to work together to find alternative ways to manage the pain and complete necessary dental work. Like having the procedure completed under sedation to keep them comfortable.
9 Causes of Trigeminal Neuralgia
Trigeminal neuralgia is typically classified into one of three categories: classical, secondary, and idiopathic (which is when they have no idea where it’s coming from.) Classical situations are usually because something like pressure or trauma is physically affecting the nerve structure. Secondary cases are when a co-existing medical condition is causing the issue, and trigeminal neuralgia is a side-effect.
Dentists and dental professionals are some of the first healthcare practitioners to see trigeminal neuralgia symptoms because they work exclusively with people’s mouths and faces. Explaining your symptoms during your dental exam—along with a bit of detective work—may lead to associating your trigeminal neuralgia symptoms with one of the following common causes of the disorder:
1. Compression of the nerve
If something is pushing down on your trigeminal nerve, it can cause pain or alter the way it functions whenever you’re trying to move your facial muscles and mouth. Compression—or being pushed between two different structures—is usually associated with some type of swelling, growth, or a neighboring blood vessel pressing up against the trigeminal nerve itself. You could also have a cyst or tumor growing in the bone and pressing against the nerve canal, causing blockage or altering nerve transmissions.
2. Multiple sclerosis
Multiple sclerosis is a chronic autoimmune disorder that affects the central nervous system, including the brain and spinal cord. The disease causes damage to the protective covering of nerve fibers, leading to the development of lesions that interfere with the transmission of nerve impulses.
Symptoms of multiple sclerosis can be variable and can include fatigue, muscle weakness, vision problems, and difficulty with balance and coordination, among others.
Trigeminal neuralgia can be associated with multiple sclerosis, as the disease can cause damage to the trigeminal nerve, resulting in irritation and pain. This can result in severe facial pain. While there is no cure for multiple sclerosis, there are treatments available that can help manage symptoms and reduce the risk of complications such as trigeminal neuralgia.
3. Brain tumors
In rare situations, brain tumors can cause trigeminal neuralgia by compressing against the trigeminal nerve. When that happens, the compression leads to irritation and damage to the nerve fibers in that area. As the tumor grows, it can place additional pressure on the nerve and surrounding tissues, resulting in a range of symptoms, including severe facial pain.
Symptoms of pain from a tumor can be intermittent or constant and may be triggered by even mild stimuli once a nerve becomes involved. In addition to pain, other symptoms of a brain tumor can include headaches, dizziness, and changes in vision or speech.
4. Arthritis
Arthritis affects the joints and is known for causing pain and inflammation. In particular, rheumatoid arthritis (RA,) which is a type of autoimmune disorder where the body attacks its own joints, can lead to chronic pain and swelling. While arthritis is typically associated with joint pain, it can also cause trigeminal neuralgia by affecting the nerves that feed the face.
In some cases, the inflammation associated with rheumatoid arthritis can lead to nerve irritation and damage, resulting in severe facial pain. If you already know that you have an autoimmune condition or RA, be sure to let your dentist know.
5. Infections or viruses
Certain types of viral infections can cause trigeminal neuralgia by irritating or damaging the trigeminal nerve.
Shingles
Shingles, for example, is a viral infection that affects nerve fibers and can cause painful rashes and blisters. In some cases, shingles can affect the nerves of the face, leading to facial pain and even trigeminal neuralgia symptoms.
Meningitis
Meningitis, a bacterial infection that affects the membranes surrounding the brain and spinal cord, can also cause facial pain and trigeminal neuralgia by causing inflammation in the nerves that supply the face.
Viral infections
While most viral infections run their course, others require specific antiviral or antibiotic medications, pain management, and in some cases, anticonvulsant medications to help manage nerve pain.
6. Stroke
A stroke can also cause trigeminal neuralgia. Strokes happen whenever there’s a sudden interruption of blood flow to the brain, which can lead to brain damage and neurological symptoms. Similar to strokes, traumatic injuries—such as car wrecks or blunt trauma—to the face or head can also cause damage to the trigeminal nerve, leading to facial pain and trigeminal neuralgia. The severity of symptoms can vary depending on the extent of the injury or stroke but can be severe and debilitating. Your physician may need to perform an MRI to determine the location and extent of the blockage so that future stroke symptoms can be avoided.
7. Tumors of the nerve
Tumors that grow on the trigeminal nerve can cause trigeminal neuralgia by pressing against and damaging the nerve fibers in that space. These tumors can be benign or malignant and can grow on or near the trigeminal nerve, leading to irritation or pain. As the tumor grows, it can also cause pressure on the nerve, leading to severe facial pain and more prominent trigeminal neuralgia symptoms.
A common example of tumor growth on nerves is caused by a condition known as neurofibromatosis type 2 (NF2.) NF2 can cause fibrous growths throughout the body, including on the skin and nerve tissues, and in some cases, may lead to trigeminal neuralgia.
8. Genetics
Trigeminal neuralgia is not generally considered a genetic or hereditary condition. Meaning it isn’t typically passed down from parent to child through genes. However, there may be some genetic factors that can increase the risk of developing the condition, including certain genetic mutations that affect the structure or function of the nerves (such as NF2, which is mentioned above.) In some cases, trigeminal neuralgia may be more common among individuals with a family history of the condition, although the exact genetic factors involved are not fully understood.
9. Idiopathic
In a lot of scenarios, trigeminal neuralgia can be idiopathic, which means that it happens without a clear cause or explanation. In many cases, idiopathic trigeminal neuralgia is thought to be related to nerve damage or irritation, although the exact mechanism is not fully understood. It is also possible that other factors, such as inflammation or infection, could be causing other issues, making trigeminal neuralgia flare up as a side-effect.
It's important to note that there may be other causes of trigeminal neuralgia and that a proper diagnosis can only be made by a medical professional. If you are experiencing facial pain, it's important to see a doctor for a proper evaluation and diagnosis.
What Triggers Trigeminal Neuralgia?
Trigeminal neuralgia (which is sometimes referred to as “tic douloureux”) is best known for the nerve pain that it causes. As with other chronic pain or neurological conditions, most people are able to identify common triggers that result in painful flareups. What is it that can irritate your nerve and make it suddenly start to hurt? While triggers can vary from one person to the next, some of the most common ones can include things like:
1. Physical stimulation
Touch or physical stimulation can sometimes trigger symptoms of trigeminal neuralgia, causing pain and discomfort in the face. This may be due to the increased pressure on the trigeminal nerve root, which can become irritated and inflamed as a result of physical contact. Activities such as brushing your teeth, chewing, or speaking may be enough to trigger painful symptoms in some individuals. Similarly, others may find that exposure to cold temperatures, such as a chilled drink or sharp gusts of wind, can also lead to a painful flareup. To manage symptoms and avoid triggers, it may be helpful to make lifestyle changes such as adjusting oral hygiene routines or avoiding extreme temperatures.
2. Cold weather
Cold weather can be a trigger for trigeminal neuralgia symptoms in some individuals. Since your trigeminal nerve is responsible for sensation in the face, and exposure to cold temperatures can cause the nerve to become inflamed or irritated, sharp drops in temperature can lead to pain and discomfort.
In some cases, the cold weather can also cause muscles to tense up, putting additional pressure on the trigeminal nerve and worsening symptoms. If you’re someone who is fairly sensitive to colder weather, consider wearing extra layers of clothing or avoiding exposure to extreme temperatures by staying indoors when possible.
3. Emotional stress
Anxiety, depression, grief, and other types of emotional stress can be a trigger for nervous system conditions like trigeminal neuralgia in some individuals. The exact mechanism is not well understood, but it is believed that stress can cause muscle tension and inflammation, which then puts pressure on the trigeminal nerve and can lead to symptoms of facial pain.
We already know that emotional stress can cause a range of physiological responses, including changes in blood pressure and heart rate or tension in your TMJ, which may contribute to trigeminal neuralgia symptoms.
4. Wind
Exposure to wind can trigger symptoms of trigeminal neuralgia in some people. Especially if the wind is harsh or it causes a drop in temperatures. Wind can lift a trampoline up in the air if it’s strong enough, so you can easily see how it might cause painful stimulation to the face with someone who has trigeminal neuralgia. Plus, there’s the chance that the wind can cause a drop in temperature, which may further aggravate the nerve and increase symptoms. Protective clothing or staying indoors on windy days is advised.
5. Touch
Touching your face, even lightly, can be painful if you have trigeminal neuralgia. When that’s the case, everything from washing your face, putting on makeup, laying your head on a pillow, or getting your teeth cleaned can hurt.
It may be that only one side of your face hurts, or you’re able to touch certain areas but not others. If you have trigeminal neuralgia, be sure to communicate closely with your dental team before and during your appointment. That way, they can adapt your care plan to ensure your comfort as best as possible.
6. Smiling or laughing
There are several different muscles around our mouth and face responsible for our facial expressions. Chances are you’re using them hundreds of times a day to talk on the phone, laugh at jokes, or just smile at someone when you cross paths. But smiling or laughing can sometimes trigger symptoms of trigeminal neuralgia in some individuals, particularly if the movement of the facial muscles puts pressure on the trigeminal nerve. The nerve may be so inflamed or irritated that it causes pain, discomfort, or spasms. To add insult to injury, not being able to smile or laugh can also interfere with your personal relationships.
7. Chewing
Surprise, surprise! Chewing, biting into, or eating food, especially harder or crunchier ones, can sometimes trigger symptoms of trigeminal neuralgia. This is because the movement in your jaw puts pressure on the trigeminal nerve, causing pain signals to travel along the nerve.
Whenever you’re chewing, your TMJ moves in all sorts of directions. When it does, it can irritate the nerve inside your head. Some types of food may be more likely to trigger symptoms than others, and not just necessarily because they require harder chewing. Cold foods and drinks, for example, may be painful and totally off-limits. And believe it or not, bananas and other high-potassium foods could possibly irritate the nerve more in people who are prone to trigeminal neuralgia.
It's important to note that triggers can vary greatly from person to person, and what triggers one person's pain may not trigger another's. It can also take time and experimentation to determine what triggers one person's pain as opposed to another’s so that they can be avoided (or at least reduced.) Knowing your triggers can be helpful as you’re working with a doctor to determine the best treatment plan.
Bananas and trigeminal neuralgia or just a common trigger?
Bananas have been identified as a potential trigger for trigeminal neuralgia in some individuals, but it’s not always the case for everyone. It’s believed that certain foods, such as those containing high levels of potassium—like bananas—can irritate the trigeminal nerve and trigger symptoms of facial pain.
However, it is important to note that triggers for trigeminal neuralgia can vary widely from person to person, and not all individuals will experience symptoms from eating bananas or other high-potassium foods. If you are experiencing symptoms of trigeminal neuralgia or are concerned about potential triggers, it is important to discuss your concerns with a healthcare professional.
Trigeminal Nerve Pain Relief
To relieve trigeminal neuralgia pain, you can take medicine, consider surgery, get injections, and make some changes in your daily life, like avoiding things that trigger the pain and keeping your mouth healthy. Trying alternative therapies and eating well can help too. Your doctor will help you figure out the best trigeminal neuralgia pain treatment plan for you because everyone's pain is different.
Talk With Your Doctor
The treatment for trigeminal neuralgia depends on the severity of the condition and the underlying cause. In some cases, medications such as anticonvulsants, muscle relaxants, or pain relievers may be used to manage pain and reduce inflammation. Other treatments may include injections of local anesthetics or steroids, nerve blocks, or physical therapy. Sometimes, trigeminal neuralgia doesn't feel like sharp, stabbing pain. Instead, it can cause a constant, dull ache, which is called "atypical trigeminal neuralgia." To figure out if you have trigeminal neuralgia, your doctor will examine and ask about your medical history to make sure it's not some other kind of facial pain.
In some cases, surgical interventions may be necessary to remove a tumor or repair damaged nerves. Alternative therapies such as acupuncture or relaxation techniques may also be helpful in managing symptoms. If you are experiencing symptoms of trigeminal neuralgia, it is important to seek medical advice from a healthcare professional who can help determine the best course of treatment for your individual needs.
Trigeminal Neuralgial Recap
Trigeminal neuralgia is a painful condition involving one of the major nerves in your head. It can be caused by injury, illness, or even a side-effect of a co-existing condition, among others. If you’re experiencing symptoms of trigeminal neuralgia, such as pain or tenderness around your face, talk to your physician or dentist about your symptoms. They may be able to prescribe medications or physical therapy to help. Knowing what your triggers are is one of the best ways to reduce painful flare-ups and uncomfortable symptoms on a day-to-day basis. With the right medical intervention, it’s possible to help treat or manage the condition to limit additional discomfort so that you can live a fairly normal life.
Make your inbox smile!
Subscribe